Effective Patient Handoffs
With large, interdisciplinary care teams, there are a lot of handoffs. How do you standardize these handoffs for smoother transitions of care? Keep reading for tips to further improve handoffs for the entire clinical team.
Effective Patient Handoffs

With large, interdisciplinary care teams, there are a lot of handoffs. How do you standardize these handoffs for smoother transitions of care? Keep reading for tips to further improve handoffs for the entire clinical team.
More Transitions Requires Better Solutions
The evolution of patient care from a solo endeavor to a team practice is undoubtedly better for the patient overall; however, the handoff continues to be a challenge for many healthcare teams. Transitioning patient information from one healthcare provider or team to another is critical for safeguarding the continuity of care, but it remains a major stumbling block for many reasons..
Transitions are happening more and more often, and despite evidence showing that communication failures occur most often during these times, we have made little progress in improving the tools we use to facilitate these processes. There have been studies characterizing what content should be in a handoff, but few, if any, studies focus on how technology can improve handoff communication.
Over 24 hours, patient responsibility may transfer 5-8 times
across 5+ physicians. Over 4,000 handoffs in care occur daily.
Communication is one of the biggest failures during handoffs. While clinicians do their best with what they have, the lack of a standardized process and collaborative tools often leaves teams relying on paper notes and outdated tech. A risky game of telephone ensues when sharing critical patient information, which can lead to errors and patient harm.
The True Cost of Poor Communication
“Our best estimates are that 150,000-250,000 patients are killed each year in the U.S. as a consequence of adverse events, which are injuries due to medical care. Communication failures contribute to 50%-80% of sentinel events. It’s the number one cause of the most serious events in hospitals, which in turn are a leading cause of death in the U.S.”
– Christopher Landrigan, MD, MPH (Boston Children’s Hospital, Principal Investigator of the I-PASS Study)
According to a malpractice risk benchmark report by CRICO, 37% of all high-severity patient injury cases – including death – involved a communication failure during provision of care. Communication failures in U.S. hospitals are estimated to have caused or contributed to 1,744 deaths and $1.7 billion in malpractice costs over five years.
Similarly, a Hospitalist Claims Study by the Doctor’s Company revealed that in 21% of claims involving improper management of treatment,communication failure among healthcare providers was the root cause.
Why Do Handoff Miscommunications Happen?
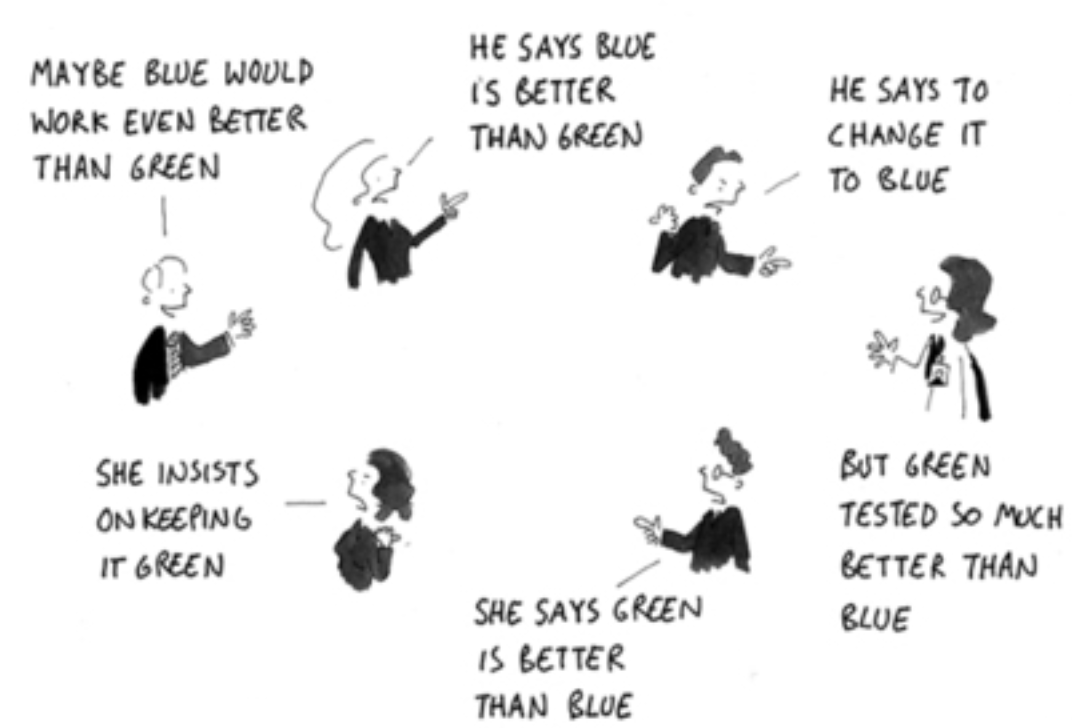
Frameworks create a foundation. But without oversight, collaboration and technology,
the process cannot be truly standardized, and errors will persist.
Lack of standardization, compounded by workplace culture and hierarchy, leads to ineffective transitions of care. Poorly-formatted written handoffs make it difficult to find information quickly, and a lack of structure in verbal handoffs causes problems with comprehension and retention.
Some organizations attempt to repurpose their existing EHR system as a solution, but the EHR is not designed for clinical workflows. Trying to force a billing and coding system to also support clinicians and patient care, particularly during already-challenging transitions, leaves much to be desired.
Gaps in handoff communication lead to situations that endanger patients and their continuity of care. There may be instances where:
-
-
- A provider communicates only the bare minimum before moving on to the next task. The person taking over will not understand the rationale behind why certain actions were or need to be taken.
- A physician sees a patient without the needed test results, so they repeat the tests or make decisions without all of the relevant information.
-
Taking Steps Towards Better Handoffs
Adverse events caused by poor communication are so prominent that, in 2006, the Joint Commission International (formerly the Joint Commission on Accreditation of Healthcare Organizations, JCAHO) introduced a national patient safety goal for handoffs. It advises healthcare organizations to standardize handoffs, and offers strategies to improve safety., given the complexity of US healthcare delivery.
The need for standardization led to recommendations such as I-PASS, SBAR and TeamSTEPPs – handoff guidelines studies which have taken on the challenge of reducing patient safety risks. The I-PASS study brought together multiple complementary interventions to improve handoff practices.
Recognizing a need to establish interdisciplinary communication, the Agency for Healthcare Research and Quality (AHRQ) developed the TeamSTEPPS toolkit. Its aim is to improve patient outcomes by focusing on communication and teamwork skills.
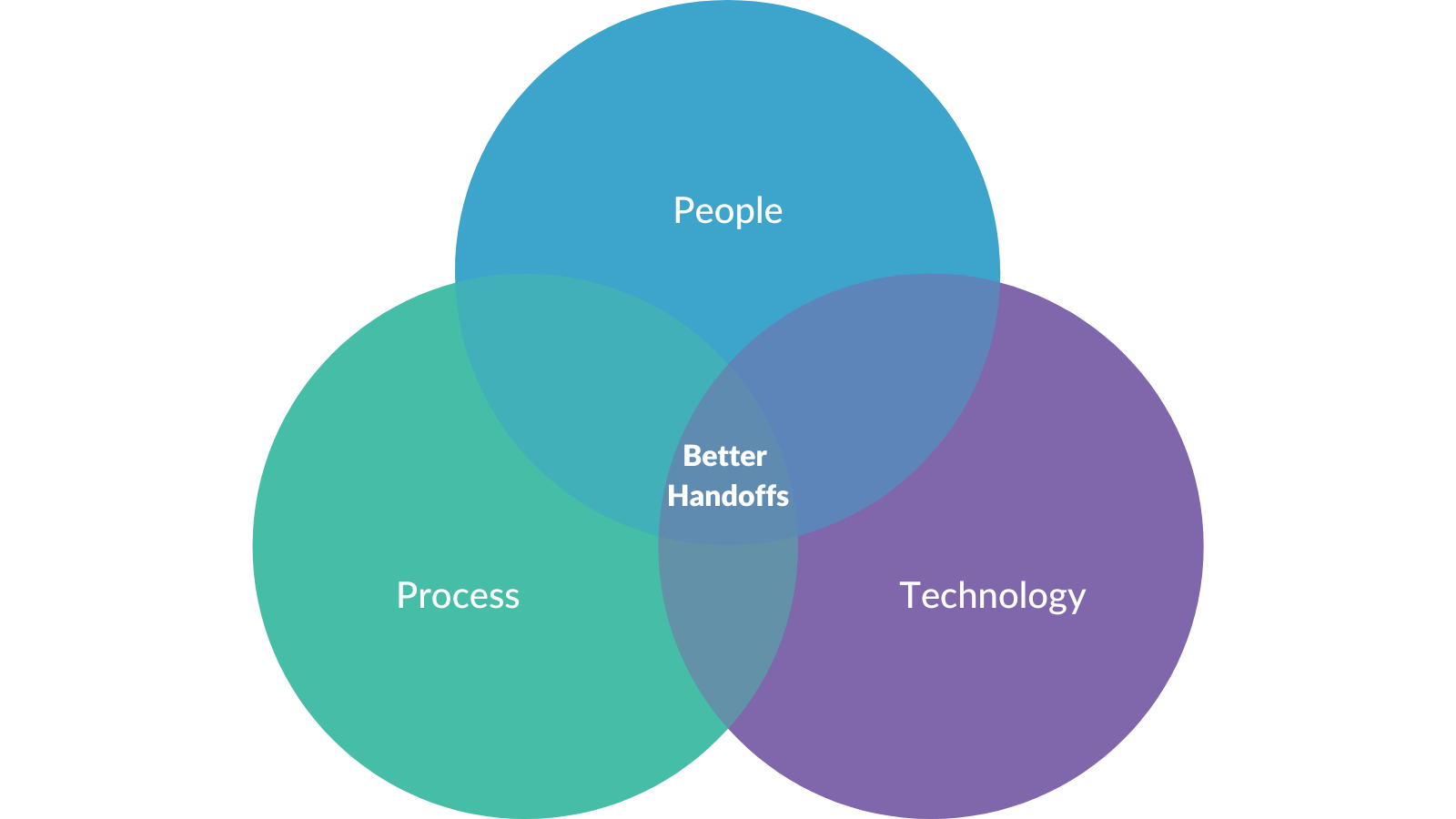
Despite their improvements, I-PASS and the TeamSTEPPS toolkit are frameworks for care teams to follow, not platforms that support interdisciplinary communication. To enable seamless communication, we must shift from process alone to process + technology + training.
ACGME partnered with the American Board of Medical Specialties (ABMS) to develop the ACGME Recommendations for Care Transitions, which mandates that programs include Team Management Milestones as a key achievement. These measure residents’ ability to transition patient care accurately and efficiently.
The ACGME, through Clinical Learning Environment Reviews (CLER), recommended common elements needed in handoffs to standardize the process:
-
-
- To-do lists
- If-then statements
- An expectation of the receiver to ask questions
- Read-backs at the end
- Clarity on when it is necessary to move to the bedside
-
For a successful handoff, clinicians should have both a written and verbal handoff. The next section will review the content, the process, and some general tips to complete a safe transition of care.
How To Create a Standardized Transition: Handoff Content

1 . Setting Expectations
Both your written and verbal handoff should start with a high level assessment of the patient, which includes:
-
-
-
- Illness/Severity assessment – is the patient sick or are you concerned their status may deteriorate?
- Code status detailing end-of-life wishes or DNR/DNI instructions.
- Main family/caregiver’s name and contact information in case of emergency and any relevant information about their level of involvement in the patient’s care.
- A concise (1- 3 sentence) assessment statement of relevant medical history and the incident that brought the patient to the hospital, i.e., the events leading up to the illness or admission, as well as current status at the time of the handoff.
- Allergies, diet, VTE prophylaxis should also be listed and easy to find in the written handoff.
-
-
2 . Patient Summary or Care Plan with Relevant Supporting Data
Most evidence recommends that handoffs include a patient summary or a list of active problems being addressed in the hospital with a short statement of the current status of the problem and treatment plan. Short enough to be able to quickly understand, but enough information to guide decision making.
For each issue, include relevant data (labs, radiology, etc). Avoid copying entire impressions or full reports, as that creates information overload, and can make it hard to read quickly. Instead, condense information into important points that summarize the findings for the next person.
Important medications should be noted, particularly recent changes in medications or doses. High risk medications to always mention include antimicrobials, anticoagulants, vasopressors, narcotics, and benzodiazepines.
3 . Tasks
Tasks that need to be done when a covering team is caring for a patient need to be clearly outlined with enough detail for the covering provider to take appropriate action.
Consider using a checklist to outline each item. Ideally these lists can be for both individual patients as well as one list of all patient tasks to ensure nothing is missed
Tasks should be specific – avoid vague language.
Provide context: Why is this task necessary? What are you looking for? What actions should be taken based on potential results?On-call teams should track what was done, what wasn’t, and any new things that were addressed overnight for handoff back to the primary team.
4 . Anticipatory Guidance
Anticipatory guidance prepares the team for scenarios that could occur in a coming shift.
Using “if-then” statements can be a powerful way to ensure the covering team has the context they need to identify what to look for and choose a course of action quickly while minimizing errors.
Contingency planning is often already written in progress notes (“if fever continues, will broaden antibiotic coverage”) – leverage this information and include it in the handoff for the on-call team.
5 . Trim and Update Information
There IS such a thing as too much information. If the covering clinicians can not quickly understand the most important points of a patient’s current status and plan, then critical decisions may be delayed. There is also evidence that paper handoffs have a short half-life and are often outdated within hours of printing, which can lead to errors. To avoid this:
-
-
-
- Clean up handoff documents regularly. Remove or archive old information that is no longer relevant (do we need the CXR from 6 days ago?).
- Ensure the information included is updated and relevant. Update symptoms and diagnoses as plans change.
-
-
Tips for the Handoff Process
Minimize Interruptions
When giving a verbal handoff, look for a quiet location and minimize interruptions. Sometimes interruptions are unavoidable – however, if they last more than ten seconds, consider restarting that patient’s verbal handoff.
Use Standard Abbreviations
Abbreviations, if used, should be common and standardized. The language and tone should be professional, without colloquialisms or slang. Speakers must be mindful of information privacy laws to avoid HIPAA violations.
Standardize Information
Standardize the order and location of information to ensure important points are not missed, and to help the receiver know what to expect. Receiving information that conforms to a known structure facilitates memory and reduces cognitive burden.
Start with a Severity Assessment
The verbal handoff should start with an illness/severity assessment. Are they sick or are you worried about them? This helps frame the rest of the patient’s information appropriately for the receiver. Even if it is in your written handoff, it is important to verbally express your concerns, such as: “This is Mrs. Jones admitted with community acquired pneumonia, who is not doing well and I’m worried about her.”

Verbal and Written Handoffs
The most effective way to communicate is to use multiple modes of information sharing to support clinicians with different learning styles (auditory vs visual). Traditionally, this means handoffs would include a face-to-face encounter plus a written handoff document. If not possible because clinicians are in different locations, handoffs should occur while viewing the same electronic document as a shared reference.
Mark Up the Text
Speakers are encouraged to use a cursor to point to or highlight items on screen, or underline text on paper. Recipients should be encouraged to update text and take notes.
Avoid Anchoring Bias
Receivers should leverage if-then statements and guidance to help with decision making, but should always make their own assessment and decisions accordingly.
Empower Receivers
Receivers should be empowered to be gently assertive and ask speakers to slow down or repeat if required. Most importantly, receivers should ask questions and repeat back key points.
Review Every Patient
It is important to review every patient on the list, even if they are stable and waiting for a test or transfer. A change in clinical status is always possible, so it is important that the covering provider knows about the patient. At a minimum, the handoff should include the patient’s name, diagnosis, status and what they are waiting for.

Questions and Read-Backs
Handoffs should have time for questions and read-backs. We comprehend and retain only 60% of what we hear, so repeating information helps with absorption. This ensures that both parties are on the same page, reducing the risk of misunderstandings that lead to errors.
The role of technology in handoffs
The main technology clinicians are given to do handoffs – and most of their other clinical work – is the EHR. The problem is, the EHRs are built for the business of healthcare, not the delivery of it. What that means is that EHRs did their initial job of digitizing paper records and helping with coding, billing, and regulatory requirements. However, these EHRs are not conducive to current clinical workflows.
Over the last two decades, the way we practice medicine has changed. Instead of one person being in charge of all the care for a patient, we have large multidisciplinary teams that work in shifts. This means that the people in charge of caring for a patient changes more frequently, leading to more handoffs.
While care has evolved to become more collaborative, our tools have not. A lot of our technology is essentially just digitized paper, leaving clinicians working in silos. So clinicians have to find different ways to collaborate about patient care – printed patient lists, daily huddles, sticky notes, emails, text messages, word documents. But these are not always good ways to communicate.

Daily huddles require everyone to be in the same place at the same time, which is not conducive to hospital at home and shift work. Emails and texts just add extra notifications that can create alert fatigue. And emails, texts, and paper can be easily lost or misplaced, meaning that information doesn’t get shared with the rest of the team.
These obstacles create an environment prone to communication breakdowns. The Joint Commission’s Sentinel Event Data 2022 Annual Review found that communication breakdowns – like not establishing a shared mental model for teams – is the leading factor contributing to sentinel events.
It is not enough to just use a pneumonic, or to teach people how to talk about handoffs. We have to give clinicians the tools they need to support these workflows and processes.
“I have always believed that technology should do the hard work – discovery, organization, communication – so users can do what makes them happiest: living and loving, not messing with annoying computers! That means making our products work together seamlessly.”
– Larry Page (Co-Founder of Google)
Key Features of Tools Needed for Good Handoffs:
Share Information Throughout the Day
These tools should facilitate information sharing throughout the whole day, not just at shift change. A good handoff tool will work across workflows – from handoffs to rounding work list and daytime scut lists – to create one task list for the patient, so the entire team can access it and see what needs to be done
Fully Functional on Mobile
Handoff tools should be fully functional on mobile devices. Clinicians should be able to access and edit patient information even if they aren’t in front of a computer. Functionality on mobile is also helpful for clinicians who see patients for home care or through telemedicine visits
Multidisciplinary
Tools should be multidisciplinary. Physicians, nurses, APPs, pharmacist, therapists, social work – we are on the same team caring for a patient. Our tools should allow us to work together. These tools should also not require sharing with specific team members so that as the patient’s care team changes, new clinicians have the information available to them right away.
Works Across Care Continuum
These tools should work across departments and care settings. Patients move to different floors or different hospitals or to skilled nursing facilities. These places may have different EHRs, but handoffs still need to happen. Handoff tools should bridge this gap to make sure the entire team can access the most up-to-date information.
Filter Tasks
Tools should have the ability to filter tasks so individuals can just view their own tasks for both an individual patient and their entire group of patients.
Assign and Schedule Tasks
Users should also be able to assign tasks to others on the clinical team with these handoff tools, and set dates and times for tasks to be done later.
Integrates into the EHR
Handoff tools should have the option to integrate into the EHR, so that the tool can bring in key clinical information that helps with decision making.
Work In Real-Time
Multiple people need to be able to view and edit the handoff tool information at the same time.
CareAlign Handoff Education
Learn more about good handoffs from Dr. Airan-Javia’s presentaton at AAIM. You can watch the full video here: https://catherinegives.org/handoff-best-practices/